People who experience ischemic stroke and arrive at the hospital quickly, as Will Shortz did, may receive one of two primary treatments: either an intravenous medication that breaks up the clot blocking a blood vessel in the brain—which is the treatment Shortz had—or, if a major artery is blocked, a procedure known as endovascular thrombectomy (or sometimes both).
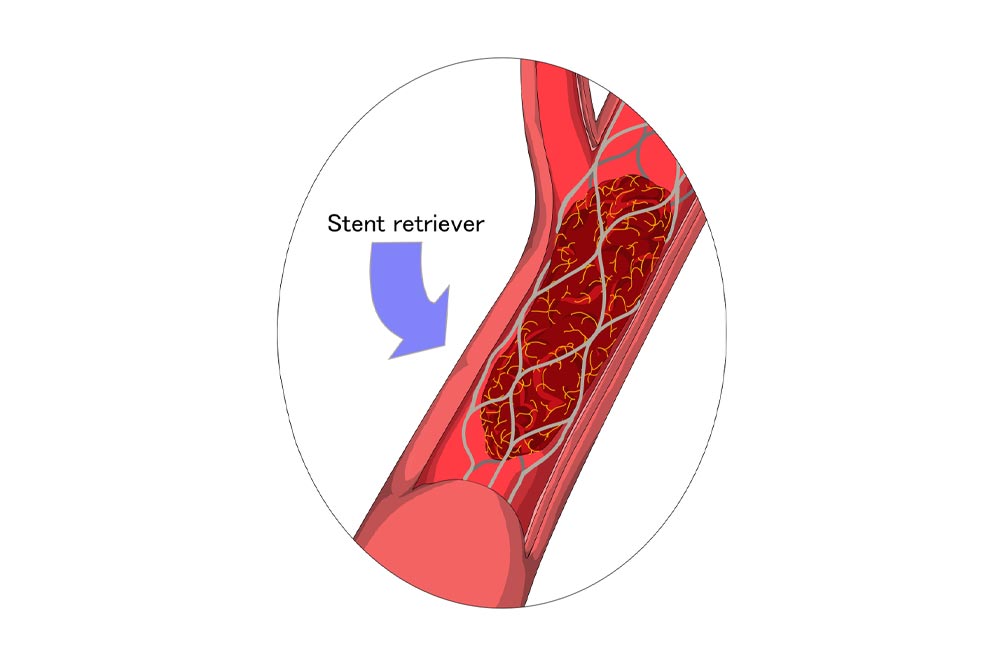
In endovascular thrombectomy, a catheter is inserted through an artery in the groin or wrist and guided up through blood vessels to the blockage in the brain. Then a stent retriever or other device captures and removes the clot, restoring blood flow.
Until recently, thrombectomy was usually not done on patients with very large core strokes (as measured by a CT scan of the brain). “For years, deciding to do thrombectomy was based only on the likelihood that we could restore the patient to independent function,” says Michael Chen, MD, professor of neurology at Rush University Medical Center in Chicago. “But that overlooked all the possible benefits to patients who otherwise would have been permanently bedbound instead of being able to get into a chair on their own or walk with assistance.”
In the SELECT2 trial, a large international study published in 2023 in the New England Journal of Medicine, patients with “large core” strokes—where large areas are affected, typically caused by blockages of the biggest vessels in the brain—were randomized to receive either endovascular thrombectomy plus medical care or medical care alone. The benefits of thrombectomy became evident so quickly that the trial was stopped early.
“Analysis of data from the study found that the procedure increased the chances of being functionally independent after one year from 6 percent to 24 percent and of being able to walk independently from 18 percent to 37 percent, without increasing the chances of bleeding into the brain,” says Larry Goldstein, MD, FAAN, endowed professor and chair of the neurology department at the University of Kentucky in Lexington. “This benefit occurred with a reduction in the risk of severe disability or death. Although the benefit is not so great as in those without evidence of irreversible brain injury, the results should be shared with patients/decision-makers when considering clot removal.”
“As the size of the stroke increased, the likelihood of improvement with thrombectomy decreased, but it still remained better than with medical care alone,” says Amrou Sarraj, MD, director of the Cerebrovascular Center and Comprehensive Stroke Center at University Hospitals Cleveland Medical Center and one of the SELECT2 lead investigators. “Five other randomized trials have shown benefits of thrombectomy in patients with large core strokes. This opens the door for a good percentage of these patients to be treated and experience benefits.”
An analysis in the Lancet in February 2024 of the SELECT2 outcomes a full year after patients’ initial strokes found continued improvements in function for the thrombectomy patients and statistically significant improvements in quality of life in areas including mobility, social relationships, cognitive function, and depression.
“A meta-analysis of six of these trials found that we were able to reduce the percentage of patients who were bedbound by half,” says Dr. Chen, citing a review in Neurology in August 2023. “That’s an incredibly powerful outcome. Patients who are bedbound are completely dependent. They get bedsores, and they are at high risk for pneumonia, urinary tract infections, and deep venous thrombosis. It just becomes an avalanche of potential health problems when you aren’t able to get up and about,” says Dr. Chen. “We have to acknowledge that most patients with a large core stroke will still have a relatively poor neurologic outcome, but it’s better with thrombectomy.”
Outcomes will be worse in patients with large core strokes than in patients with smaller strokes, but there are still benefits, agrees Sara Rostanski, MD, assistant professor of neurology at NYU Grossman School of Medicine and medical director of the stroke program at Bellevue Hospital Center in New York City. “Almost every time thrombectomy has been studied since the seminal trials in 2016, we’ve seen positive results. But if a stroke is not properly identified early on, patients have less chance of benefiting from these treatments,” says Dr. Rostanski. “I can’t emphasize enough the importance of acting immediately if someone shows signs of stroke, such as sudden numbness or weakness in the face, arms, or legs, especially if it’s on one side; sudden trouble walking or dizziness; or sudden confusion or difficulty in speaking or understanding speech. Knowing those signs and calling 911 are the most important things anyone can do to improve the chances of recovery from stroke.”